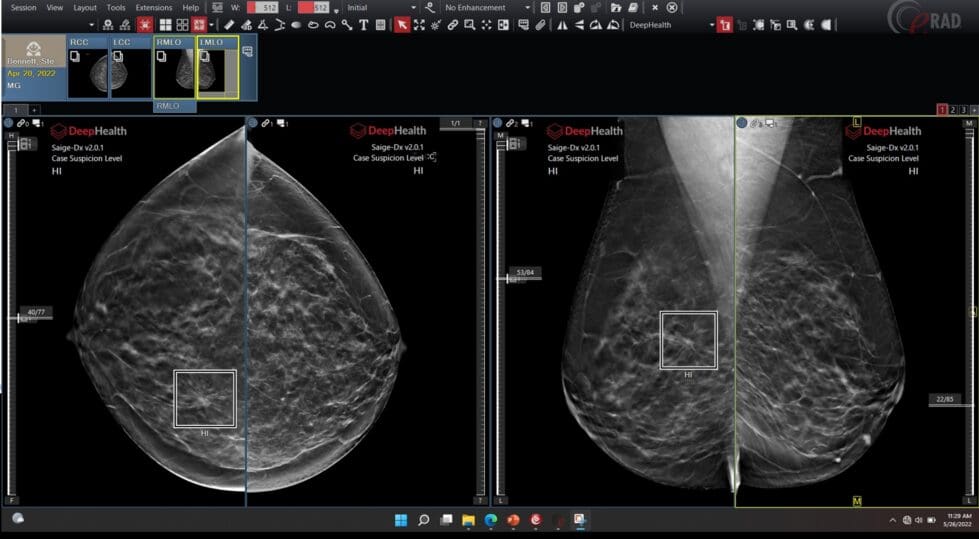
This mammogram from Delaware Imaging Network shows how artificial intelligence has flagged areas of concern for radiologists to consider.
The use of artificial intelligence in screening for breast cancers and a little used technique that can efficiently and economically find cancers in women at high risk for that cancer are among the topics to be tackled during the Delaware Breast Cancer Coalition’s annual update in May.
Dr. Jacqueline Holt, medical director of the Delaware Imaging Network, says that AI has helped radiologists find more cancers when they are smaller and more curable.
AI software trained on millions of images of breast scans is spotting and flagging subtle cancers for radiologist to review, and helping reduce the number of patient callbacks for additional imaging.
Dr. Diana Dickson-Witmer, a breast surgical oncologist with Beebe Healthcare, plans to continue spreading the word at the update about a screening technique called contrast enhanced mammography that can help find breast cancer in high-risk patients at a cost far less than the current typical MRI scan now used to look.
The technique has been approved by the Federal Food and Drug Administration for 12 years, but is not routinely used simply because there’s not a single billing code to use for it, she said.
Contrast enhanced mammography also has the potential to expand access for screening for women who need it, she said.


Dr. Jacqueline Napoletano Holt
What’s new in mammograms and advanced breast cancer detection is one of five focus topics in the 16th annual Breast Cancer Update, which will revolve around a theme of conquering the unknown while rising above a breast cancer diagnosis.
Other topics will include the differences between post mastectomy options of reconstruction or no reconstruction; hospice and palliative care support options for patients and their loved ones; the benefits of mental health and cancer survivorship therapy programs; and alternatives available for breast reconstruction, nipple creation, and artistic expression with tattooing.
The update will take place from 7:30 a.m. to 1 p.m. May 15 online and in person with a viewing party at Goldey-Beacom College in Pike Creek. It’s free. To attend, register here.
The update typically draws breast cancer patients and survivors, their families, physicians, nurses, students and allied health professionals.
“Our goal is to have programming that empowers our community in the fight against breast cancer,” the coalition website said. “The Annual Breast Cancer Update allows us to bring nationally renowned speakers in the breast cancer field and allows us to educate the community about the innovative research, treatment and programs that are available in Delaware.”
AI and mammograms
Finding cancer when it’s small pays off in lives saved, Holt said.
“When a breast cancer is found early, the survival is 99% in Stage 1,” meaning it has not started spreading. Holt said.
“Even when there’s a lymph node positive or regional disease, the survival rate approaches 90%,” she said. “And it’s not just the survivability but the hope is to decrease the amount of surgery, such as lumpectomies instead of mastectomies, unless chemotherapy or sometimes no chemotherapy at all is needed.”
The use of artificial intelligence has risen dramatically since the COVID-19 pandemic started, breast cancer specialists say.
“The challenges of reading screening mammograms are that multiple cancers can present very subtly,” Holt said. “They can bury themselves or be obscured by dense breast tissue and also the number of images, especially since we went to uniformly using 3D mammograms or digital breast tomosynthesis. Sometimes there’s 100 images embedded in each field, which leads to a complexity, a lot for the radiologists to handle.”
Delaware Imaging Network uses AI software from DeepHealth. The software is exposed to many more kinds of cancer than a typical breast radiologist would see in a career, Holt said.
“AI is trained on cancer just like AI is trained on facial recognition,” she said. “So it’s trained on seeing the face of cancer. It’s not reading the mammograms. It is augmenting and assisting and making the radiologist better and finding more cancers with the help of AI.”
The software program will flag spots for a radiologist to check, she said. If it’s suspicious, a second radiologist also will examine the scan to help determine whether a patient has cancer or needs additional screening.
Since her network began using DeepHealth in 2022, Holt says it’s identified cancer in about 400 patients that it previously might have missed, almost all of it early and curable. The network doesn’t have statistics on that yet because patients need to be followed for years.
AI is particularly good at spotting things such as subtle calcifications – which can be a precursor to cancer — on the edges of a scan or buried in dense tissue, she said.
Holt will show graphs in her talk on May 15 that illustrate how the program has helped every radiologist who used it catch cancers that might have been missed.
“AI has helped us find all different kinds of cancers, the aggressive ones, the early ones, so it’s across the board,” Holt said. “It’s not like it’s just finding cancers that don’t matter, if you will. It’s helping us find aggressive as well as, you know, the less aggressive cancers.”
Contrast enhanced mammography


Dr. Diana Dickson-Witmer
Dickson-Witmer says the aspect of artificial intelligence in mammography that she’s most excited about is the possibility that as it evolves, it one day may be able to help predict whether cancer will develop in a breast.
Dickson-Witmer right now is focused on spreading the word about contrast enhanced mammography.
The procedure involves intravenously injecting a contrast material into a woman’s bloodstream and doing a mammogram that takes a series of images of the breasts.
Breast cancers grow their own blood vessels, but they’re leaky. The contrast material will begin to leach into surrounding tissue within moments and that spread will be caught on the scans, Dickson-Whitmer said.
Healthcare facilities shy away from the procedure because it requires a series of billing codes that cover the use of the machine as well as the injection of the contrast material, among other things, she said.
Dickson-Whitmer is part of a coalition of breast specialists promoting the technique, including Dr. Constance Lehman, a professor of radiology at Harvard Medical School who works at Mass General in Boston, Massachusetts.
One of the benefits of the technique is that it uses the less expensive mammography machine rather than the much more expensive magnetic resonance imaging machine.
It’s particularly important because the guidelines for who should be considered at high risk for the development of breast cancer was expanded significantly in May 2023, Dickson-Whitmer said.
The category includes women who have dense breasts, may have had cancer before and those in many other situations.
Millions of breast exams
“So we’re now talking about millions and millions of women for which high risk screening with MRI is recommended,” Dickson-Whitmer said. “Well, that would break the bank.”
Healthcare facilities can’t afford to use their MRIs for that many scans, and doing so could mean that less money is put into prevention programs, she said.
Most facilities usually have a digital mammography machine, she said.
“It’s about $160,000 needed for the software for the training and hardware to upgrade a digital mammogram machine to be able to do contrast enhanced mammography,” she said.
A new MRI is $1.5 million to $3 million, she said. Each MRI screening costs the system about $5,000 simply for its use as opposed to about $600 for contrast enhanced mammography, she said.
“There’s just orders of magnitude difference in cost and therefore in access,” she said.
2024 Update sessions
7:30 a.m. Registration & Sponsor Exhibits
8:20 a.m. Session I Mammography & AI
Moderator: Dr. Renee Quarterman
Dr. Diana Dickson Witmer
Dr. Jacqueline Holt
9:20 a.m. Session II Reconstruction or
No Reconstruction Post Mastectomy
Moderator: Dr. Karen Louie
Dr. Dawn Leonard
Dr. Stephanie Caterson
10:30 a.m. Session III Hospice and Palliative Care
Moderator: Dr. Wendy Newell
Dr. Avani Virani
Dr. Dan DePietropaolo
11:10 a.m. Session IV Mental Health Wellness
Moderator: Dr. Matt Richards
Dr. Chalice Rhodes
12:10 p.m. Session V Tattooing & Cosmetic Options
Moderator: Connie Holdridge
Mandy Sauler
Survivor testimonials


Betsy Price is a Wilmington freelance writer who has 40 years of experience, including 15 at The News Journal in Delaware.
Share this Post