ChristianaCare Scientists Advance CRISPR Research Against Drug-Resistant Cancer
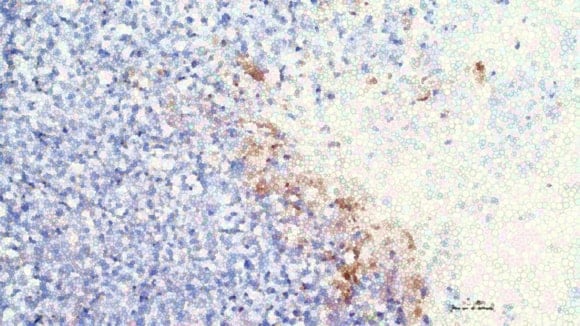
ChristianaCare’s Gene Editing Institute used CRISPR to reverse chemotherapy resistance in a common form of lung cancer by targeting a key survival gene. (Photo courtesy of ChristianaCare.)
ChristianaCare’s Gene Editing Institute says it has found a way to reverse chemotherapy resistance in one of the most common forms of lung cancer, using a CRISPR-based approach that disables a key gene known to help tumors survive treatment.
The findings, published Nov. 13 in Molecular Therapy Oncology, show that disrupting the NRF2 gene restored sensitivity to standard chemotherapy drugs and slowed tumor growth in both human lung cancer cell lines and animal models, according to the research team.
“We’ve seen compelling evidence at every stage of research,” said Kelly Banas, Ph.D., lead author of the study and associate director of research at the Gene Editing Institute. “It’s a strong foundation for taking the next step toward clinical trials.”
Focus on a Hard-to-Treat Lung Cancer
The study examined lung squamous cell carcinoma, an aggressive subtype of non-small cell lung cancer that accounts for up to 30% of cases nationwide. The American Cancer Society estimates that more than 190,000 people in the U.S. will be diagnosed with lung cancer this year.
While the work centered on this specific cancer, the researchers said the approach may apply more broadly. Overactive NRF2 is known to drive chemotherapy resistance in several solid tumors, including liver, esophageal, and head and neck cancers.
“This is a significant step toward overcoming one of the biggest challenges in cancer therapy – drug resistance,” Banas said. “By targeting a key transcription factor that drives resistance, we’ve shown that gene editing can re-sensitize tumors to standard treatment.”
Targeting a “Master Switch”
Scientists zeroed in on a mutation called R34G in the NRF2 gene. When hyperactive, NRF2 acts like a “master switch” that helps cancer cells withstand chemotherapy. Using CRISPR/Cas9, the team engineered lung cancer cells with the mutation and then knocked out the gene, restoring their response to carboplatin and paclitaxel.
In animal studies, tumors treated directly with the CRISPR therapy also showed slower growth and improved response to chemotherapy.
“This work brings transformational change to how we think about treating resistant cancers,” said Eric Kmiec, Ph.D., senior author and executive director of the Gene Editing Institute. “Instead of developing entirely new drugs, we are using gene editing to make existing ones effective again.”
Partial Editing Still Showed Results
Researchers reported that editing just 20% to 40% of tumor cells was enough to enhance chemotherapy’s effectiveness—an important finding for potential clinical use, where reaching every cancer cell is unlikely.
For delivery, the team used lipid nanoparticles, a non-viral method increasingly viewed as a safer, more precise alternative to older gene-therapy vehicles. Sequencing results showed minimal off-target effects.
“The power of this CRISPR therapy lies in its precision. It’s like an arrow that hits only the bullseye,” Banas said. “This level of specificity with minimal unanticipated genomic side effects offers real hope for the cancer patients who could one day receive this treatment.”
The Gene Editing Institute expects future studies to explore whether the approach can be tested in early-phase clinical trials.
RELATED STORIES:

Sara Uzer is a journalist from Sussex County with more than 15 years of experience as a writer, editor, and community advocate. She started her career in Washington, DC and has lived in Sussex County for the past five years.
Share this Post









